The promise of modern healthcare often falls short for people who live far from major medical centers. In rural and underserved communities, millions struggle to reach specialists, wait too long for primary care, and go without consistent medical support.
The result is predictable.
Health outcomes decline, chronic conditions worsen, and already thin local resources are pushed to the breaking point.
A shift is finally taking shape.
A new wave of telehealth startups is using practical technology such as secure video visits, AI assisted diagnostics, and remote monitoring tools to remove long standing barriers to care.
These companies are not simply offering online appointments. They are reshaping the delivery of healthcare so rural patients can access timely, high quality medical support from home or through their local clinics.
The Challenge: Closing the gap in rural healthcare
Rural regions face a shortage of medical professionals in nearly every specialty, a growing population of older adults who need more care, and internet infrastructure that often lags behind.
Patients must travel long distances and spend money they do not have, which leads many to delay treatment until conditions worsen. The traditional system was never built to serve such spread out communities.
Telehealth must rise to the task by providing comprehensive and dependable care, not just simple video calls.
This means building technology that works in low bandwidth environments and delivering care with the patience and understanding that rural communities deserve.
Hazel Health
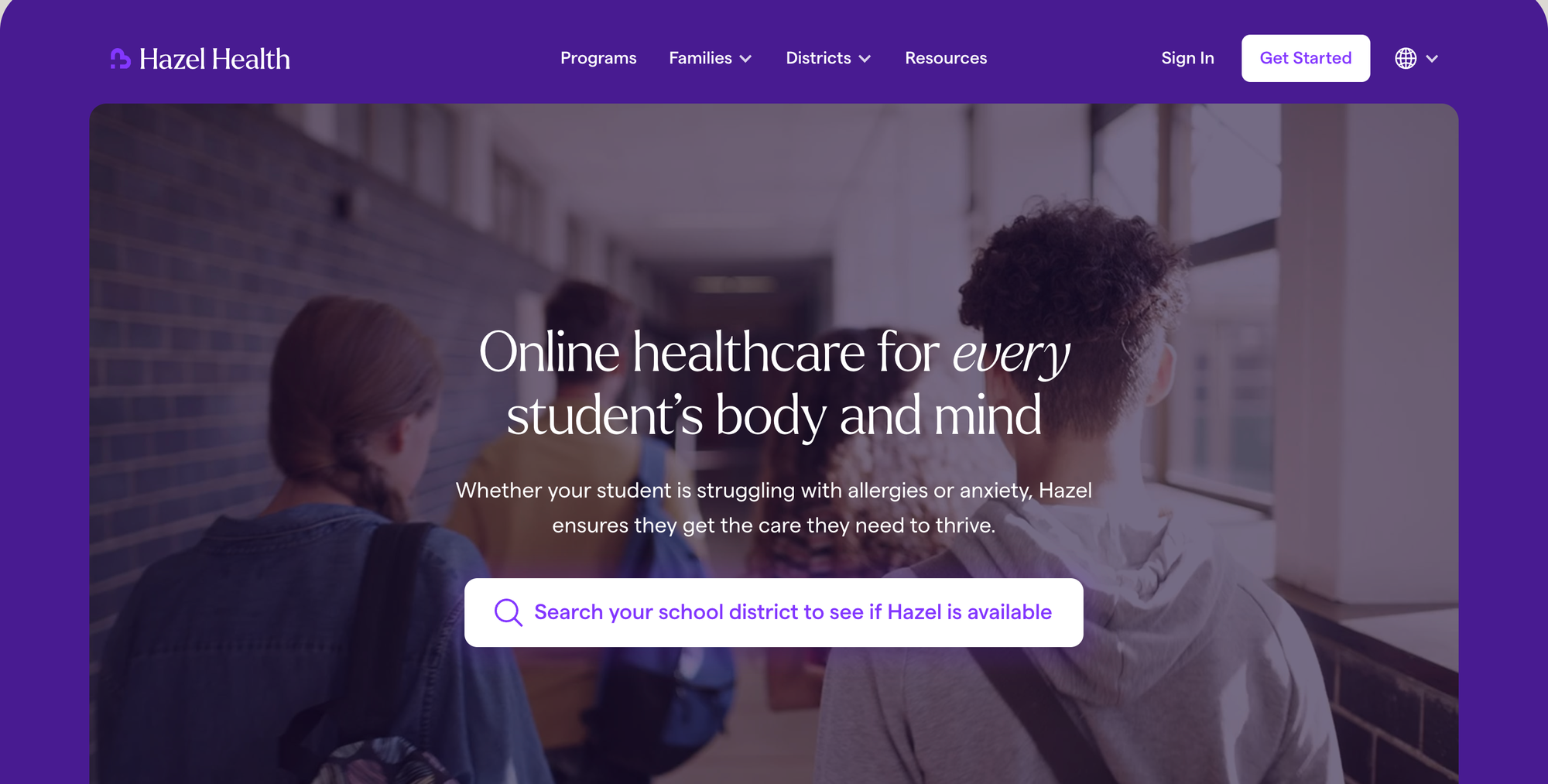
- Core Innovation: Specializes in providing pediatric and mental health services directly within K-12 public schools through a video platform.
- Impact on Rural Access: School nurses in rural districts often serve as the main point of health access for children. Hazel connects these schools to licensed pediatric specialists and mental health therapists, ensuring that children receive immediate care and support without parents needing to miss work or drive long distances to a clinic.
- Key Data Point: Serves schools across over 10 states, acting as a vital health gateway for thousands of rural students.
SteadyMD
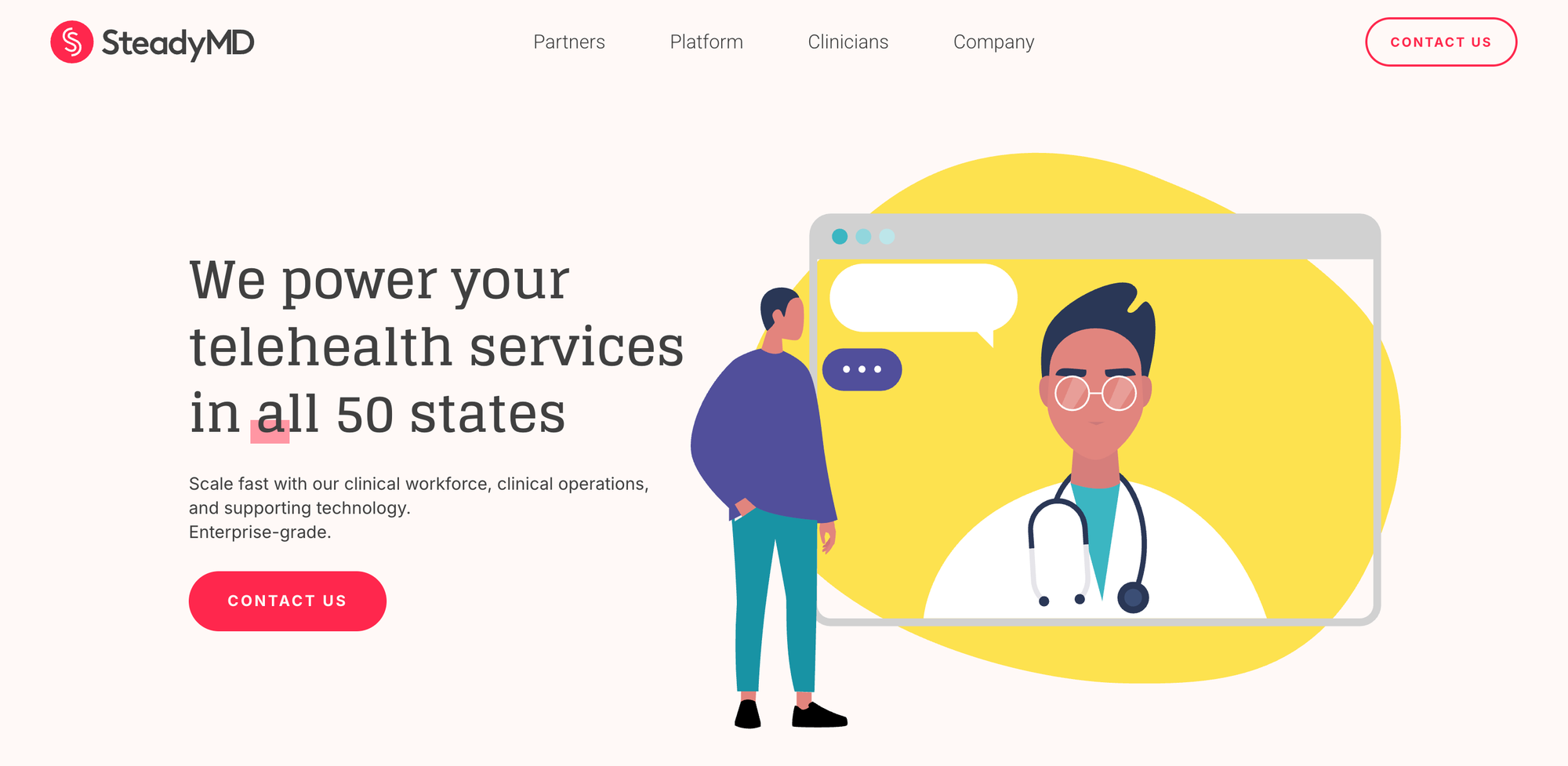
- Core Innovation: Provides full service virtual care infrastructure, including clinician staffing, credentialing support, and clinical operations for organizations that want to offer telehealth without building internal teams.
- Impact on Rural Access: Gives rural clinics and health systems a simple way to expand telehealth without major overhead. This strengthens access to primary care, urgent care, and chronic care management for communities that often lack consistent staffing.
- Key Data Point: SteadyMD supports nationwide clinical coverage across all 50 states, which allows rural providers to scale services immediately.
Equip Health
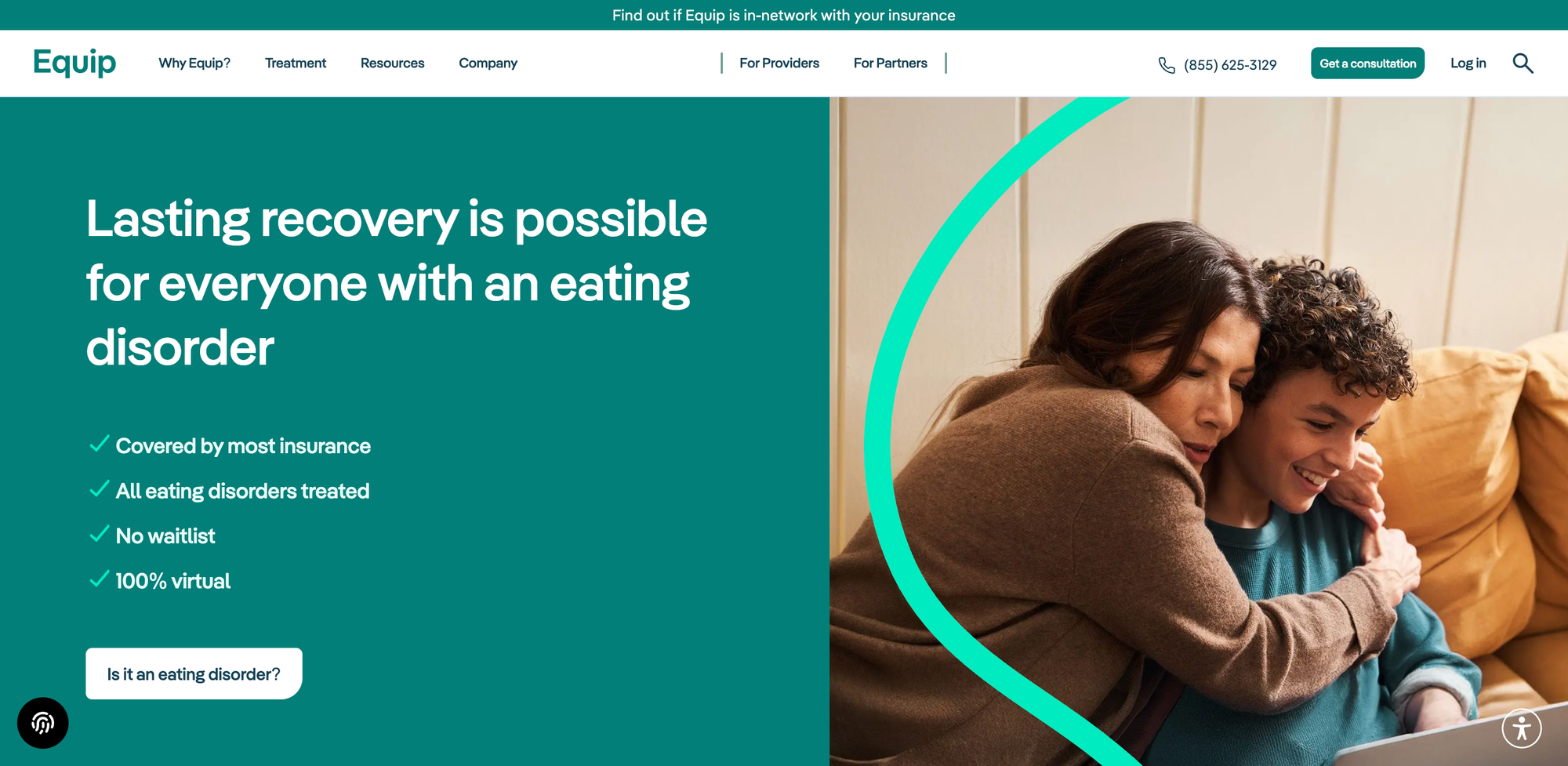
- Core Innovation: Delivers virtual eating disorder treatment through a coordinated care team. Services include therapy, nutrition support, peer mentorship, and medical oversight delivered entirely through telehealth.
- Impact on Rural Access: Rural families rarely have eating disorder specialists close by. Equip replaces long travel requirements with a complete care model available at home, which increases early intervention and improves adherence to treatment.
- Key Data Point: Equip reports significantly higher completion rates than traditional in person programs, largely due to easier access and family based care.
Wheel
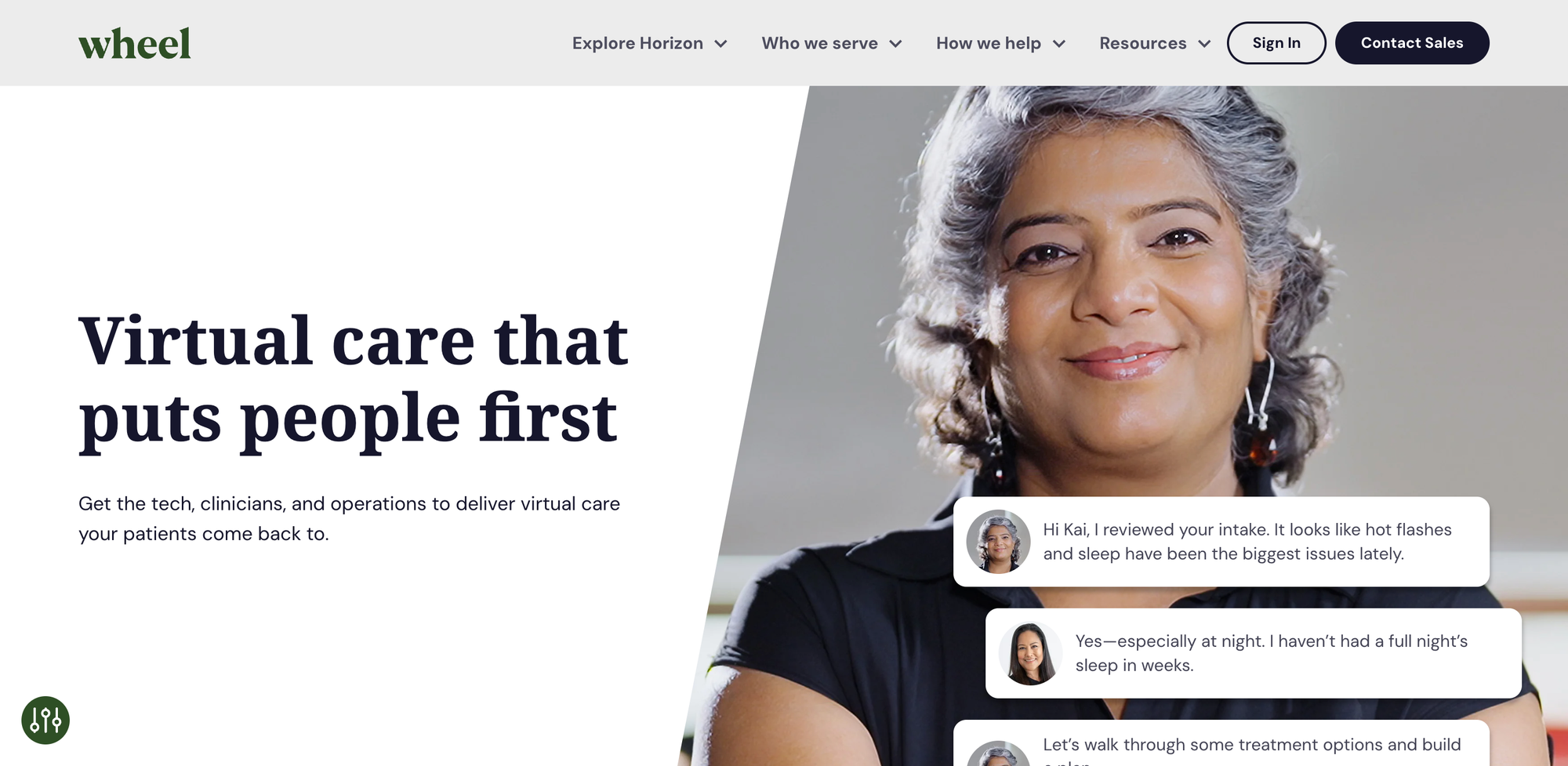
- Core Innovation: An asynchronous and synchronous virtual care platform that connects healthcare companies with a vetted network of clinicians. Wheel acts as the infrastructure for other companies to build their virtual care offerings.
- Impact on Rural Access: By streamlining the deployment of virtual care services, Wheel indirectly expands rural access by enabling more healthcare providers and innovators to launch telehealth programs quickly and efficiently, staffing them with qualified professionals.
- Key Data Point: Powers virtual care for over 100 enterprise clients, dramatically expanding the reach of telehealth.
Hone Health
- Core Innovation: A telehealth platform specializing in hormone optimization and longevity (e.g., testosterone replacement therapy, menopause care). Care is driven by advanced lab testing (40+ biomarkers) and physician consults, with treatments shipped directly to the patient.
- Impact on Rural Access: Addresses highly specialized and often difficult-to-access therapies for aging and hormone imbalances, which require consistent lab work and follow-up—services that are scarce in rural settings. Hone brings the entire process, including testing logistics, to the patient's home.
- Key Data Point: Offers testing across 40+ biomarkers, providing a deeper data-driven view of patient health for personalized treatment plans.
TytoCare
- Core Innovation: Develops a handheld, at-home physical examination device that allows users to perform comprehensive exams (heart, lungs, skin, ears, throat, abdomen) with data streamed live to a clinician for remote diagnosis.
- Impact on Rural Access: Transforms basic video consultations into near-in-person examinations. This is crucial for rural patients, enabling accurate, remote diagnoses for acute conditions (like ear infections or strep throat) that typically require a physical visit, eliminating unnecessary travel to the nearest clinic or ER.
- Key Data Point: Their device is FDA-cleared and significantly enhances the diagnostic capabilities of virtual care platforms globally.
Mindstrong Health
- Core Innovation: Focuses on mental health, using digital phenotyping (passive, continuous measurement of smartphone interaction patterns) combined with telehealth to detect and manage mental health conditions earlier.
- Impact on Rural Access: Provides discreet, accessible, and continuous mental health support to rural individuals who often face significant stigma and extremely limited access to in-person psychiatric services.
- Key Data Point: Their technology aims to provide objective mental health measurements to complement clinical assessments.
Brave Health
- Core Innovation: A virtual mental health clinic offering comprehensive individual and group therapy, and personalized medication management for a wide range of conditions (e.g., anxiety, depression, bipolar disorder, PTSD). Crucially, they accept most insurance plans, including Medicaid and Medicare.
- Impact on Rural Access: Directly addresses the severe shortage of mental health professionals in rural and underserved areas. By focusing on patients covered by Medicaid and Medicare, Brave Health makes high-quality, continuous mental healthcare affordable and accessible to low-income and elderly rural populations who often have the greatest difficulty finding local providers.
- Key Data Point: Delivers care via secure video sessions and reports significant symptom improvement, with 2 out of 3 patients with depression seeing symptoms improve after one month of treatment.
Oshi Health
- Core Innovation: A virtual clinic dedicated to inflammatory bowel disease (IBD) care. Oshi provides integrated care from gastroenterologists, dietitians, and behavioral therapists through a comprehensive virtual platform.
- Impact on Rural Access: For complex chronic conditions like IBD, specialist access in rural areas is exceptionally difficult. Oshi brings highly specialized, multidisciplinary care directly to patients' homes, improving disease management and quality of life.
- Key Data Point: Demonstrated significant reduction in IBD-related emergency department visits for their members.
Brightside Health
- Core Innovation: A virtual mental health platform offering personalized psychiatry and therapy for mild-to-severe anxiety and depression, including a first-of-its-kind national program for elevated suicide risk. Uses AI to analyze 100+ data points for precision medication prescribing.
- Impact on Rural Access: Directly tackles the critical shortage of mental health professionals and addresses the high-risk, high-acuity cases often underserved by general telehealth platforms, providing fast access to evidence-based care in all 50 states.
- Key Data Point: Claims 75% of patients achieve remission within 12 weeks, significantly outperforming traditional care models.
Ophelia
- Core Innovation: Provides virtual medication assisted treatment for opioid use disorder, pairing clinicians with digital tools that support ongoing counseling, follow up visits, and care navigation.
- Impact on Rural Access: Rural regions often have high overdose rates and very few treatment centers. Ophelia gives patients confidential, continuous treatment without traveling long distances, which increases enrollment and retention.
- Key Data Point: Patients using Ophelia show strong retention in treatment, which is one of the most important predictors of long term recovery.
Key Technology Trends Analysis
The innovation from these telehealth startups highlights critical shifts in healthcare delivery:
- Specialized & High-Acuity Care: Telehealth is increasingly moving beyond urgent care to address complex, chronic, mental health, and specialized conditions (like hormone optimization), where specialist shortages are most acute in rural settings.
- AI-Driven Precision: Startups like Brightside Health are using AI and machine learning to analyze patient data for clinical decision support, moving from generalized prescribing to personalized, evidence-based treatment, which is essential when a local doctor isn't available for continuous monitoring.
- Hybrid Care Models: The convergence of virtual and physical care is becoming the standard, ensuring that telehealth complements rather than replaces local clinical resources, particularly in rural areas.
- Continuous Remote Monitoring: Integration of IoT medical devices allows for continuous, proactive patient management for chronic conditions, transforming reactive care into preventive and personalized interventions.
Wrapping Up
The digital revolution in healthcare is rapidly closing the geographical gaps that have long defined rural access to care.
The telehealth startups highlighted here are not merely offering convenience; they are building the essential infrastructure and services that guarantee equitable access to quality medical attention, regardless of zip code.
By leveraging innovative technologies and patient-centric models, they are fundamentally strengthening the health and well-being of rural communities, proving that the future of healthcare is both virtual and universally accessible.







